
ADVANCE CARE PLANNING: Begin Exploring | Choices / What Matters | New Paths | Choose Agent
Create Directive | Share | Store-Revise | Peace & Grace
Your Personal Values for a Meaningful Quality of Life
 Think about what matters most to you in your care at the end of life. Talking it over with friends and loved ones, exploring information and ideas together, can help you answer some essential questions. Writing your choices in a Personal Values statement is essential.
Think about what matters most to you in your care at the end of life. Talking it over with friends and loved ones, exploring information and ideas together, can help you answer some essential questions. Writing your choices in a Personal Values statement is essential.
In the past this statement has been separate from an Advance Directive. It is now either incorporated into an Advance Directive or attached to it as a definitive guide.
Listen to Journalist Ellen Goodman Talk About
The Most Important Ongoing Conversations You Can Have
Listen to this TED Talk by journalist Ellen Goodman as she describes what happened at the end of her mother’s life and how we might go about making our choices.
Deciding What Matters Most to You
Here are a few questions you might consider:
If things went well for you at the end of your life what would doing well in your last days look like?
What if you no longer had the ability to recognize and interact with loved ones?
Is maintaining personal mobility and dignity important to you?
Is there any type of music you like to hear?
Are there any circumstances where you would consider life to be not worth living?
Where would you want to be when you die?
Who would you like to have around you at that time?
If you become seriously ill, do you wish complete honesty about your condition and your prognosis for recovery from your physician(s), care providers and family?
Do you want to know how a recommended treatment will affect the quality of your life after a treatment or procedure?
Would you want to have the support of Palliative Care team to manage your symptoms and pain if you have a long term, life-limiting disease or condition?
Do you want the support of a Hospice Care team for yourself and your family if you have a terminal illness and it is thought that you have six months or less to live?
If you have a terminal disease are there any circumstances when you might be willing to consider the options of palliative sedation, voluntary stopping of eating and drinking, medical aid in dying?
Talking With Friends and Loved Ones
 The Conversation Project
The Conversation Project
Founded by Ellen Goodman, The Conversation Project began in 2010, when she and a group of colleagues and concerned media, clergy, and medical professionals gathered to share stories of “good deaths” and “bad deaths” within their own circle of loved ones. The organization is dedicated to helping people talk about their wishes for end of life care. It provides multiple resources to enable these conversations.
Begin “Your Conversation”
Answer questions in this guide to help you think about what matters most to you at the end of your life. Talk with others to learn their views.
Download your free Conversation Starter Kit by clicking HERE
 Go Wish Cards
Go Wish Cards
Another tool to get you started in thinking about what matters most to you in an end of life situation. Each card asks a question, you have to place that card in one of three categoriesL Very important; Somewhat important; or Not important. Doing this is more difficult than you think. Since you must limit the Very important category to ten, you have to prioritize. Here is an example of a “card” – To Have know me as a whole person. You can play this “card” game online or purchase set(s) to play with friends and family at home.
 Hello – A Conversation Game
Hello – A Conversation Game
Hello is a conversation game. It’s the easy, non-threatening way to start a conversations with your family and friends about living and dying and what matters most toy.
 Consider the Conversation Award Winning film
Consider the Conversation Award Winning film
Watch this film with your family and friends to help start conversations on important issues. A film fostering communication between between husband and wife, doctor and patient, minister and parishioner, parent and child. A film about living to the fullest up to the very end of our days.
Video on Vimeo
Also available as a DVD HERE
 Advice for Future Corpses *(and Those Who Love Them):
Advice for Future Corpses *(and Those Who Love Them):
A Practical Perspective on Death and Dying
by Sallie Tisdale
Former NEA fellow and Pushcart Prize-winning writer Sallie Tisdale offers a lyrical, thought-provoking, yet practical perspective on death and dying Informed by her many years working as a nurse, with more than a decade in palliative care. Tisdale explores all the heartbreaking, beautiful, terrifying, confusing, absurd, and even joyful experiences that accompany the work of dying, including:
Good Death: What does it mean to die “a good death”? What can I do to make my death, or the deaths of my loved ones, good?
Communication: What to say and not to say, what to ask, and when, from the dying, loved ones, doctors, and more.
Last Months, Weeks, Days, and Hours: What you might expect, physically and emotionally, including the limitations, freedoms, pain, and joy of this unique time.
Bodies: What happens to a body after death? What options are available to me after my death, and how do I choose—and make sure my wishes are followed?
Grief: “Grief is the story that must be told over and over…Grief is the breath after the last one.”
Find it in your local library or Order it online
Understanding Hard Choices
Meet a Leader for Change in End of Life Care
Jessica Nutik-Zitter, MD
 Extreme Measures
Extreme Measures
Finding a Better Path to the End of Life
Jessica Nutik-Zitter, MD
This remarkably caring physician takes us on a journey of understanding how the high-intensity procedures in an ICU that can save the lives of younger people often put elders on a “conveyor belt” of invasive and painful treatments that leave us tethered to machines – unnecessarily prolonging our suffering and robbing us of the possibilities for peace and dignity at the end of our lives. Dr Zitter compassionately suggests a different model of knowledge, choice and communication between patients, families and care givers.
Find the book at a library or order it online
Extremis – streaming video
A documentary available for streaming on Netflix Directed and produced by Dan Krauss.
Watch this documentary to understand what happens in an intensive care unit. A short Netflix original documentary film, nominated for a 2016 Academy Award, Extremis follows Jessica Nutik-Zitter MD in an intensive care unit as she and other doctors consider critical end of life care decisions and communicate the difficult choices to patients and families.
Available for streaming – Enter Extremis in the search field on the Netflix.com website.
Emergency Medical Treatments in an ICU
What Does “Full Code” or “Full Treatment” Mean?
In the US medical system, when a person is admitted to an Intensive Care Unit in life-threatening condition they will be given what is know as “full code” or “full treatment”, in other words all the treatment measures that you see in the video Extremis or are described in the book Extreme Measures by Jessica Nutik-Zitter described below. One treatment often requires another in a cascade of invasive, stressful, and sometimes painful treatments. Some treatments, such as intubation (life sustaining breath support with connection to a ventilator) have a time frame. It can only used for roughly two weeks before a decision needs to be made about whether to remove or to continue permanent breathing assistance by surgically inserting a breathing tube through a hole in the throat. When this is done a patient is permanently connected to a breathing tube /ventilator and must live on life support in a “sub-acute” care facility for the rest of their life. Learn about this type of care in An Impossible Choice video described below.
Find more information about Full Treatment in an ICU in the Serious Illness section of this site.
More Help in Understanding Care Choices
 Hard Choices for Loving People
Hard Choices for Loving People
CPR, Feeding Tubes, Palliative Care,
Comfort measures, and the Patient with a Serious Illness
by Hank Dunn M. Div.
A small book to help navigate some of the difficult health care decisions for people with serious illnesses or facing end of life choices.
Find the book at a library or order it online
 Choices at the End of Life
Choices at the End of Life
Finding Out What Your Parents Want before It’s Too Late
by Linda Norlander RN,MS and Kristin McSteen RN, M
A very helpful overview of the process of advance care planning and end of life care situations for adult children trying to engage their parents in a kitchen table conversation about future care.
Find the book at a library or order it online
An Impossible Choice
Deciding When a Life is No Longer Worth Living
 VIDEO – An Impossible Choice
VIDEO – An Impossible Choice
Deciding When a Life is No Longer Worth Living
A though-provoking video by Joanne Faryon, photos and video by Brad Racino
A powerful documentary which deals with the dilemmas of living on long term life-support in a sub-acute care facility. The video outlines the medical milestones and emotion-filled choices that lead to the withdrawing of life support. Other helpful support videos are available on this site.
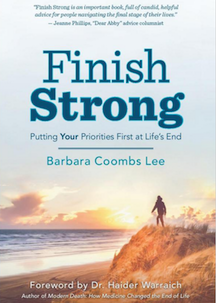 Finish Strong: Putting Your Priorities First at Life’s End
Finish Strong: Putting Your Priorities First at Life’s End
by Barbara Coombs Lee
Written by a nurse, physician assistant and attorney who is a leading advocate for end of life options, this book describes concrete action in the here and now to help live our best lives to the end. It guides the reader through: finding a partner-doctor to honor your values and beliefs with humanity, deference and candor; identifying what matters most as vigor wanes; stating your priorities; having meaningful conversations with doctors and family about expectations and wishes, staying off the “over-treatment conveyor belt.”
Find it in your local library or Order it online.
 On Our Own Terms
On Our Own Terms
Bill Moyers – two DVD set of the PBS Series
An emotional and constructive look at how our culture faces death, renowned journalist Bill Moyers interviews dozens of terminally ill patients. From a gentle pediatrician who chooses not to combat his cancer with chemotherapy to palliative-care doctors and hospice workers who focus on comfort rather than cure, this four-part program uses individual portraits to explain the complex concepts and choices that surround “a good death.”
Find it at a local library or Order it online
Choosing Support & Peace at the End of Life
Part of the advance care planning process is understanding the significant value of incorporating both Palliative Care and Hospice Care into your future care plans. Learn how each of these services can bring you and your family peace at the end of your life.
It will be very helpful if you talk with your family now about your desire to engage these services at the appropriate time and to indicate your preferences for this type of care in your advance directive. There are full sections on this site that describe these fine services.
Learn about Palliative Care
Learn about Hospice Care
Dying Matters – streaming documentary
The Dying Matters Coalition is led by the National Council for Palliative Care, the umbrella charity for end of life care in England, Wales and Northern Ireland.. The Coalition’s Mission is to help people talk more openly about dying, death and bereavement, and to make plans for the end of life. Wide selection of films. Watch it here
End of Life Options
There are a few options, some controversial and some not available everywhere, that a person with a terminal illness may consider to hasten their expected death in order to avoid prolonged pain and suffering that no longer responds to treatment. It is essential that these options be explored only in consultation with your primary care physician, spiritual advisors and loved ones.
The information is presented below is provided solely as a matter of education on each topic.
Each individual must make his/her personal choices in consultation with any and all health professionals involved in his/her care.
VSED – Voluntary Stopping of Eating and Drinking
Palliative Podcasts:
Voluntary Stopping of Eating and Drinking
An informative a podcast from Stanford School of Medicine relating to a Journal of American Geriatrics Society article, March 2018
Find the podcast here
Dying Wish
A documentary film about hospice patient, Dr. Michael Miller, an eighty-year old, retired surgeon with end-stage cancer who chooses to stop eating and drinking in order not to prolong his dying process, to ease his suffering and to die with grace.
Learn more
Palliative Sedation – Sedation to Unconsciousness
Terms you might hear in discussing this option:
Refractory pain or refractory symptoms, caused by advanced stages of a serious illness,. Pain that does not yield to increasing levels of treatment.
Titration describes the process of adjusting the standard dosage of a medication up or down based on an individual patient’s reactions.
Some sources for understanding this option:
Palliative Sedation: Myth vs. Fact by the Center to Advance Palliative Care
Statement on Palliative Sedation
American Academy of Palliative and Hospice Medicine
Hard Choice for a Comfortable Death: Sedation
by Anemone Hartocollis – article -New York Times
Medical Aid in Dying (MAiD) – the End of Life Options Act
Physician-Assisted death or Medical Aid in Dying is legal in ten jurisdictions: California, Colorado, District of Columbia, Hawaii, Montana, Maine (starting January 1, 2020), New Jersey, Oregon, Vermont, and Washington. The legislation that provides for Medical Aid in Dying may be titled differently depending on the state that passes the legislation. It may be called the End of Life Options Act, the Death with Dignity Act, the Aid in Dying for the Terminally Ill Act; etc. Essentially, each Act permit a mentally competent person diagnosed with a terminal illness who has less than six months to live to seek the assistance of a physician who may prescribe a drug combination that will end their life. The factor that distinguishes Medical Aid in Dying from Euthanasia is that the patient must administer the drug to them selves without assistance from the physician or others. Medical Aid in Dying is a process accomplished over a set of conditions carried out over a time frame in consultation with medical professionals.
Four Discussions and Points of View
The following articles, each written by a caring physicians, explore the dilemma of evolving state legislation that permits terminally ill patients to help determine how long they will live if they have a seriously debilitating disease or physical conditions, and acute or intractable pain.
Physician-Assisted Suicide Won’t Atone for Medicine’s ‘Original Sin’
by Ira Byock, MD – article in STAT News
Read the article
I’m a Doctor With End-Stage Cancer. I Support Medical Aid in Dying
by Roger Kligler – article in STAT News
Read the article
Should I Help My Patients Die?
by Jessica Nutik-Zitter – article New York Times
Read the article
How Not to Die
by Angelo Valances – article in The Atlantic
Read the article
Speaking of Dying – Living Deeply, Dying Well
Watch the trailer here
The 30-minute documentary captures the voices and stories of people becoming comfortable speaking of dying. Many of those you will meet in the film have overcome their fears and found comfort through their participation in the pioneering, community-based workshops of chaplain Trudy James and her Heartwork partners. You will also meet medical professionals who speak candidly about the importance of planning and discussing your plans with others. Find it here
Organizations to Help You Learn More
about End of Life Choices
Compassion & Choices
Compassion & Choices is the nation’s oldest, largest and most active nonprofit organization committed to improving care and expanding options for the end of life. The organization seeks to improves care and expands options for the end of life. It supports, educates and advocates nationwide in state legislatures, Congress, courts, medical settings and communities to ensure healthcare providers honor and enable patients’ decisions about their care. Learn More
Death With Dignity
A non-profit organization founded and based in Oregon, Death with Dignity National Center has a mission to promote Death with Dignity laws, (also known as Medical Aid in Dying or End of Life Options Act) based on the Oregon model legislation both to provide an option for dying individuals; to stimulate nationwide improvements in end-of-life care;and to expand the freedom of all qualified terminally ill Americans to make their own end-of-life decisions, including how they die. Learn more
Center for Ethics
The OHSU Center for Ethics envisions health care that is compassionate, just and respectful for the people of Oregon and across the nation. The center is dedicated to combining the ethical perspectives of health care professionals, patients and families to improve teaching, research, and clinical consultation in patient care and health policy. The center also advocate for institutional and public policies that promote ethical goals in health care services and systems.
Learn more
End of Life Washington
The organization supports personal rights to the full range of end of life choices, including Death with Dignity, through advocacy, education, and support. End of Life Washington is recognized nationally for its advocacy of choice for the terminally ill and its commitment to improved treatment of pain and other symptoms. Learn more
Euthanasia
Euthanasia is the controversial personal decision to end one’s life through assisted suicide. It is different from Medical Aid in Dying (see above).